 Book Appointment
Book Appointment
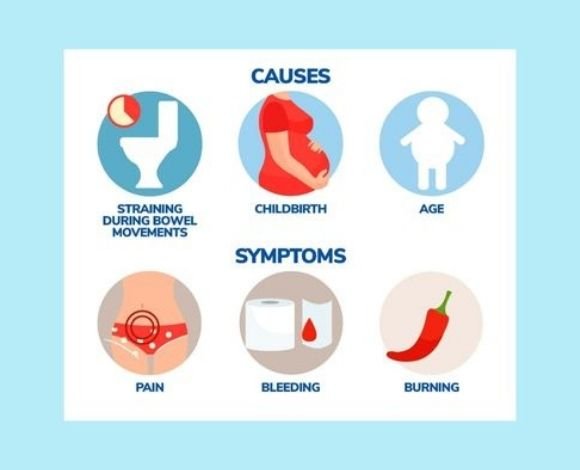
Anal fissures may sound minor, but anyone who has suffered from one knows how painful and disruptive they can be. Even the simple act of passing stools can feel like “passing glass,” leaving patients anxious, fearful, and avoiding bowel movements altogether. Many people silently struggle with anal fissures, often misdiagnosing them as piles (hemorrhoids). While early fissures sometimes heal with home remedies and lifestyle changes, chronic fissures (lasting beyond 6–8 weeks) often need surgical treatment for permanent relief.
The good news is that with modern techniques like Laser Fissure Surgery and Lateral Internal Sphincterotomy (LIS), treatment today is safe, quick, minimally invasive, and highly effective.
At our surgical practice, we combine:
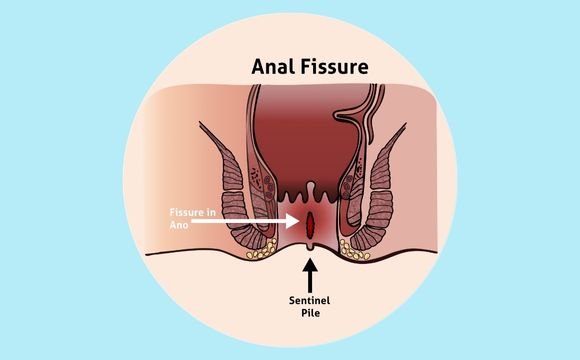
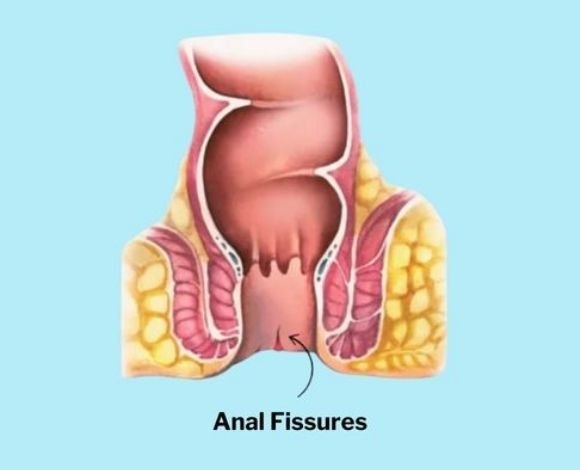
An anal fissure is a small tear in the thin, moist lining (mucosa) of the anus. Though tiny, the tear exposes sensitive tissue and nerves, leading to severe pain, bleeding, and muscle spasms. Many patients describe the pain as sharp, burning, or cutting, which can last for hours after a bowel movement.

Early treatment is crucial to prevent the fissure from becoming chronic and harder to treat.
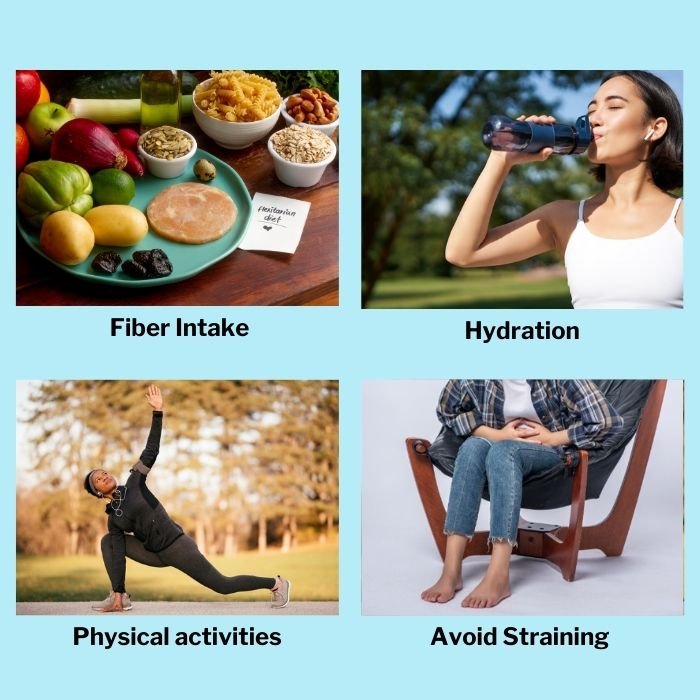
Most acute fissures (less than 6 weeks old) respond well to conservative care.
If these methods fail after 6–8 weeks, or if fissures keep recurring, surgery is recommended.
Modern surgical advancements have transformed fissure treatment — moving away from painful open procedures to safer, day-care, minimally invasive options. Below is the difference between laser and LIS for fissure, helping patients understand which procedure may be more suitable for their condition.
General Guidelines:

Fissure surgery is very safe, but like any procedure, risks may include:
With an experienced surgeon, these risks are minimized.
The cost of anal fissure surgery varies based on:
Patient Information Guide